
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
- Mi-kyung Kim
- Diabetes Metab J. 2021;45(6):968-969. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0311
- 2,609 View
- 65 Download
- Drug/Regimen
- Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
- Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Kim, Hye Soon Kim, Il Seong Nam-Goong, Eun Sook Kim, Jin Ook Chung, Dong-Hyeok Cho, Chang Won Lee, Young Il Kim, Dong Jin Chung, Kyu Chang Won, In Joo Kim, Tae Sun Park, Duk Kyu Kim, Hosang Shon
- Diabetes Metab J. 2021;45(5):675-683. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0107
- 35,350 View
- 367 Download
- 9 Web of Science
- 5 Crossref
-
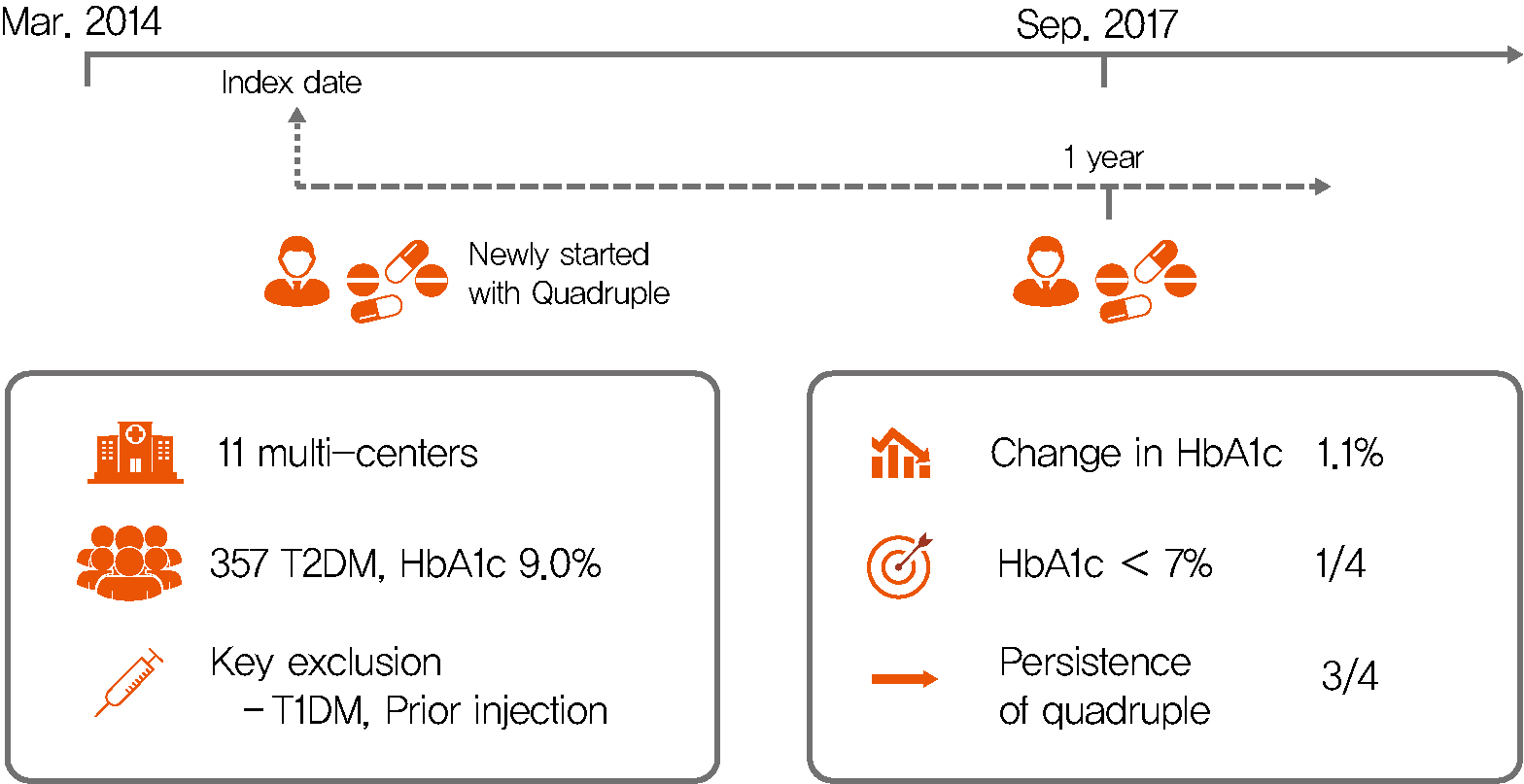
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 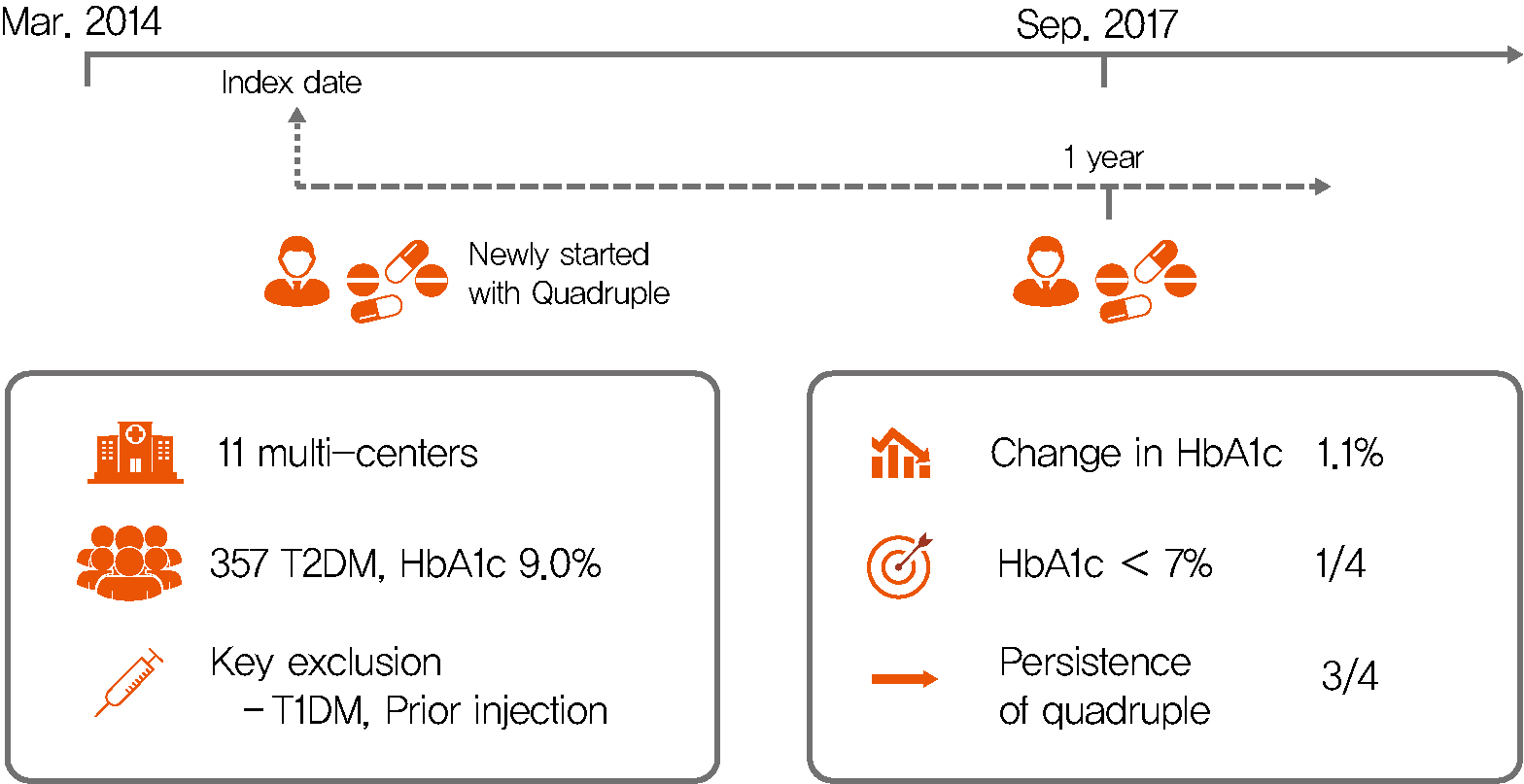
Background Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%;
P <0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P <0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.Conclusion This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
-
Citations
Citations to this article as recorded by- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
Rita Oliveira, Matilde Monteiro-Soares, José Pedro Guerreiro, Rúben Pereira, António Teixeira-Rodrigues
Pharmacy.2024; 12(1): 18. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef
- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
- Letter: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (
Diabetes Metab J 2019;43:879–92) - Mi-kyung Kim
- Diabetes Metab J. 2020;44(1):203-204. Published online February 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0018
- 3,290 View
- 60 Download
- Epidemiology
- Low-Normal Free Thyroxine Levels in Euthyroid Male Are Associated with Prediabetes
- Sung Woo Kim, Jae-Han Jeon, Jun Sung Moon, Eon Ju Jeon, Mi-Kyung Kim, In-Kyu Lee, Jung Beom Seo, Keun-Gyu Park
- Diabetes Metab J. 2019;43(5):718-726. Published online March 19, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0222
- 4,321 View
- 51 Download
- 2 Web of Science
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Abnormal thyroid function is associated with impaired glucose homeostasis. This study aimed to determine whether free thyroxine (FT4) influences the prevalence of prediabetes in euthyroid subjects using a cross-sectional survey derived from the Korea National Health and Nutrition Examination Survey, conducted between 2013 and 2015. We studied 2,399 male participants of >20 years of age who were euthyroid and non-diabetic. Prediabetic participants had lower FT4 concentrations than those without prediabetes, but their thyrotropin concentrations were similar. We stratified the population into tertiles according to FT4 concentration. After adjusting for multiple confounding factors, glycosylated hemoglobin (HbA1c) levels significantly decreased with increasing FT4 tertile, whereas fasting plasma glucose (FPG) levels were not associated with FT4 tertiles (HbA1c,
P <0.01 in T3 vs. T1; FPG,P =0.489 in T3 vs. T1). The prevalence of prediabetes was significantly higher in T1 (odds ratio, 1.426; 95% confidence interval, 1.126 to 1.806;P <0.01) than in T3. In conclusion, subjects with low-normal serum FT4 had high HbA1c and were more likely to have prediabetes. These results suggest that low FT4 concentration is a risk factor for prediabetes in male, even when thyroid function is within the normal range.
- Epidemiology
- Insulin Resistance versus β-Cell Failure: Is It Changing in Koreans?
- Mi-kyung Kim
- Diabetes Metab J. 2018;42(2):128-129. Published online April 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.128
- 2,976 View
- 31 Download
- 3 Web of Science
- 3 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- β-hydroxybutyrate as a biomarker of β-cell function in new-onset type 2 diabetes and its association with treatment response at 6 months
Minyoung Lee, Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes & Metabolism.2023; 49(4): 101427. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Effects of Y1 receptor agonist on the pancreatic islet of diet-induced obese and diabetic mice
Priscila Viana Carapeto, Carlos A. Mandarim-de-Lacerda, Marcia Barbosa Aguila
Journal of Diabetes and its Complications.2020; 34(9): 107669. CrossRef
- β-hydroxybutyrate as a biomarker of β-cell function in new-onset type 2 diabetes and its association with treatment response at 6 months
- Clinical Care/Education
- Patient Understanding of Hypoglycemia in Tertiary Referral Centers
- Nan Hee Cho, Nam Kyung Kim, Eugene Han, Jun Hwa Hong, Eon Ju Jeon, Jun Sung Moon, Mi Hae Seo, Ji Eun Lee, Hyun-Ae Seo, Mi-Kyung Kim, Hye Soon Kim
- Diabetes Metab J. 2018;42(1):43-52. Published online February 23, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.1.43
- 4,585 View
- 54 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypoglycemia is an important complication in the treatment of patients with diabetes. We surveyed the insight by patients with diabetes into hypoglycemia, their hypoglycemia avoidance behavior, and their level of worry regarding hypoglycemia.
Methods A survey of patients with diabetes, who had visited seven tertiary referral centers in Daegu or Gyeongsangbuk-do, Korea, between June 2014 and June 2015, was conducted. The survey contained questions about personal history, symptoms, educational experience, self-management, and attitudes about hypoglycemia.
Results Of 758 participants, 471 (62.1%) had experienced hypoglycemia, and 250 (32.9%) had experienced hypoglycemia at least once in the month immediately preceding the study. Two hundred and forty-two (31.8%) of the participants had received hypoglycemia education at least once, but only 148 (19.4%) knew the exact definition of hypoglycemia. Hypoglycemic symptoms identified by the participants were dizziness (55.0%), sweating (53.8%), and tremor (40.8%). They mostly chose candy (62.1%), chocolate (37.7%), or juice (36.8%) as food for recovering hypoglycemia. Participants who had experienced hypoglycemia had longer duration of diabetes and a higher proportion of insulin usage. The mean scores for hypoglycemia avoidance behavior and worry about hypoglycemia were 21.2±10.71 and 23.38±13.19, respectively. These scores tended to be higher for participants with higher than 8% of glycosylated hemoglobin, insulin use, and experience of emergency room visits.
Conclusion Many patients had experienced hypoglycemia and worried about it. We recommend identifying patients that are anxious about hypoglycemia and educating them about what to do when they develop hypoglycemic symptoms, especially those who have a high risk of hypoglycemia.
-
Citations
Citations to this article as recorded by- Severe Hypoglycemia Increases Dementia Risk and Related Mortality: A Nationwide, Population-based Cohort Study
Eugene Han, Kyung-do Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Seung-Hyun Ko, Yong-ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(5): e1976. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Response: Patient Understanding of Hypoglycemia in Tertiary Referral Centers (Diabetes Metab J 2018;42:43-52)
Nan Hee Cho, Hye Soon Kim
Diabetes & Metabolism Journal.2018; 42(2): 175. CrossRef - Letter: Patient Understanding of Hypoglycemia in Tertiary Referral Centers (Diabetes Metab J 2018;42:43-52)
Jae-Han Jeon
Diabetes & Metabolism Journal.2018; 42(2): 173. CrossRef
- Severe Hypoglycemia Increases Dementia Risk and Related Mortality: A Nationwide, Population-based Cohort Study
- Corrigendum: Author ORCID Number Correction. Dietary Sodium Intake in Patients with Type 2 Diabetes Mellitus
- Mi-Kyung Kim
- Diabetes Metab J. 2017;41(1):79-79. Published online February 16, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.1.79
- 2,482 View
- 27 Download
- Others
- Repeated Glucose Deprivation/Reperfusion Induced PC-12 Cell Death through the Involvement of FOXO Transcription Factor
- Na Han, You Jeong Kim, Su Min Park, Seung Man Kim, Ji Suk Lee, Hye Sook Jung, Eun Ju Lee, Tae Kyoon Kim, Tae Nyun Kim, Min Jeong Kwon, Soon Hee Lee, Mi-kyung Kim, Byoung Doo Rhee, Jeong Hyun Park
- Diabetes Metab J. 2016;40(5):396-405. Published online September 1, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.5.396
- 4,670 View
- 30 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cognitive impairment and brain damage in diabetes is suggested to be associated with hypoglycemia. The mechanisms of hypoglycemia-induced neural death and apoptosis are not clear and reperfusion injury may be involved. Recent studies show that glucose deprivation/reperfusion induced more neuronal cell death than glucose deprivation itself. The forkhead box O (FOXO) transcription factors are implicated in the regulation of cell apoptosis and survival, but their role in neuronal cells remains unclear. We examined the role of FOXO transcription factors and the involvement of the phosphatidylinositol 3-kinase (PI3K)/Akt and apoptosis-related signaling pathways in PC-12 cells exposed to repeated glucose deprivation/reperfusion.
Methods PC-12 cells were exposed to control (Dulbecco's Modified Eagle Medium [DMEM] containing 25 mM glucose) or glucose deprivation/reperfusion (DMEM with 0 mM glucose for 6 hours and then DMEM with 25 mM glucose for 18 hours) for 5 days. MTT assay and Western blot analysis were performed for cell viability, apoptosis, and the expression of survival signaling pathways. FOXO3/4',6-diamidino-2-phenylindole staining was done to ascertain the involvement of FOXO transcription factors in glucose deprivation/reperfusion conditions.
Results Compared to PC-12 cells not exposed to hypoglycemia, cells exposed to glucose deprivation/reperfusion showed a reduction of cell viability, decreased expression of phosphorylated Akt and Bcl-2, and an increase of cleaved caspase-3 expression. Of note, FOXO3 protein was localized in the nuclei of glucose deprivation/reperfusion cells but not in the control cells.
Conclusion Repeated glucose deprivation/reperfusion caused the neuronal cell death. Activated FOXO3 via the PI3K/Akt pathway in repeated glucose deprivation/reperfusion was involved in genes related to apoptosis.
-
Citations
Citations to this article as recorded by- Predictive factors for the development of diabetes in cancer patients treated with phosphatidylinositol 3-kinase inhibitors
Gyuri Kim, Myungeun Yoo, Min Hee Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Hye Ryun Kim, Yong-ho Lee, Byoung Chul Cho
Cancer Chemotherapy and Pharmacology.2019; 84(2): 405. CrossRef
- Predictive factors for the development of diabetes in cancer patients treated with phosphatidylinositol 3-kinase inhibitors
- Epidemiology
- Dietary Sodium Intake in Patients with Type 2 Diabetes Mellitus
- Mi-Kyung Kim
- Diabetes Metab J. 2016;40(4):280-282. Published online August 18, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.4.280
- 3,492 View
- 46 Download
- 8 Web of Science
- 7 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Effects of different diets on glycemic control among patients with type 2 diabetes: A literature review
Maryam E Al-Adwi, Zinab M Al-Haswsa, Karmen M Alhmmadi, Yasmin A Eissa, Aya Hamdan, Hiba Bawadi, Reema F Tayyem
Nutrition and Health.2023; 29(2): 215. CrossRef - Effects of dietary salt intake restriction on blood glucose levels: a meta-analysis of crossover study
Yong Shen, Yujie Shi, Jiajing Cui, Haitao He, Shuping Ren
Nutrition Research and Practice.2023; 17(3): 387. CrossRef - Association of sodium intake with diabetes in adults without hypertension: evidence from the National Health and Nutrition Examination Survey 2009–2018
Li Ming, Duan Wang, Yong Zhu
Frontiers in Public Health.2023;[Epub] CrossRef - Fatores associados ao consumo de sal na população adulta brasileira: Pesquisa Nacional de Saúde
José Geraldo Mill, Deborah Carvalho Malta, Eduardo Augusto Fernandes Nilson, Ísis Eloah Machado, Patrícia Constante Jaime, Regina Tomie Ivata Bernal, Laís Santos de Magalhães Cardoso, Célia Landman Szwarcwald
Ciência & Saúde Coletiva.2021; 26(2): 555. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef - Multilayered Interplay Between Fructose and Salt in Development of Hypertension
Ozgur C. Eren, Alberto Ortiz, Baris Afsar, Adrian Covic, Masanari Kuwabara, Miguel A. Lanaspa, Richard J. Johnson, Mehmet Kanbay
Hypertension.2019; 73(2): 265. CrossRef - Novel paradigms linking salt and health
M Popovic, R Velicki, Lj Torovic, J Bjelanovic, J Janjic, R Mitrovic, M Z Baltic
IOP Conference Series: Earth and Environmental Science.2019; 333(1): 012036. CrossRef
- Effects of different diets on glycemic control among patients with type 2 diabetes: A literature review
- Complications
- Renoprotective Effect of Gemigliptin, a Dipeptidyl Peptidase-4 Inhibitor, in Streptozotocin-Induced Type 1 Diabetic Mice
- Gwon-Soo Jung, Jae-Han Jeon, Mi Sun Choe, Sung-Woo Kim, In-Kyu Lee, Mi-Kyung Kim, Keun-Gyu Park
- Diabetes Metab J. 2016;40(3):211-221. Published online March 31, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.211
- 6,345 View
- 53 Download
- 22 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase-4 (DPP-4) inhibitors are widely used in the treatment of patients with type 2 diabetes and have proven protective effects on diabetic kidney disease (DKD). Whether DPP-4 inhibitors have renoprotective effects on insulin-deficient type 1 diabetes has not been comprehensively examined. The aim of this study was to determine whether gemigliptin, a new DPP-4 inhibitor, has renoprotective effects in streptozotocin (STZ)-induced type 1 diabetic mice.
Methods Diabetes was induced by intraperitoneal administration of a single dose of STZ. Mice with diabetes were treated without or with gemigliptin (300 mg/kg) for 8 weeks. Morphological changes of the glomerular basement membrane (GBM) were observed by electron microscopy and periodic-acid Schiff staining. In addition, we measured blood glucose and urinary albumin excretion and evaluated fibrotic markers using immunohistochemical staining, quantitative reverse transcription polymerase chain reaction analysis, and Western blot analysis.
Results Gemigliptin did not reduce the blood glucose levels of STZ-treated mice. In gemigliptin-treated mice with STZ, a significant reduction in urinary albumin excretion and GBM thickness was observed. Immunohistological examination revealed that gemigliptin attenuated renal fibrosis induced by STZ and decreased extracellular matrix protein levels, including those of type I collagen and fibronectin, and Smad3 phosphorylation. In cultured rat renal cells, gemigliptin inhibited transforming growth factor β-stimulated type I collagen and fibronectin mRNA and protein levels via down-regulation of Smad3 phosphorylation.
Conclusion Our data demonstrate that gemigliptin has renoprotective effects on DKD, regardless of its glucose-lowering effect, suggesting that it could be used to prevent DKD, including in patients with type 1 diabetes.
-
Citations
Citations to this article as recorded by- Diabetic fibrosis
Izabela Tuleta, Nikolaos G. Frangogiannis
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2021; 1867(4): 166044. CrossRef - Protective roles of thymoquinone and vildagliptin in manganese-induced nephrotoxicity in adult albino rats
Heba El-Sayed Mostafa, Eman Ahmed Alaa El-Din, Dalia Abdallah El-Shafei, Nehal S. Abouhashem, Aisha Abdallah Abouhashem
Environmental Science and Pollution Research.2021; 28(24): 31174. CrossRef - Evogliptin, a Dipeptidyl Peptidase-4 Inhibitor, Attenuates Renal Fibrosis Caused by Unilateral Ureteral Obstruction in Mice
Mi-Jin Kim, Na-young Kim, Yun-A Jung, Seunghyeong Lee, Gwon-Soo Jung, Jung-Guk Kim, In-Kyu Lee, Sungwoo Lee, Yeon-Kyung Choi, Keun-Gyu Park
Diabetes & Metabolism Journal.2020; 44(1): 186. CrossRef - Gemigliptin Attenuates Renal Fibrosis Through Down-Regulation of the NLRP3 Inflammasome
Jung Beom Seo, Yeon-Kyung Choi, Hye-In Woo, Yun-A Jung, Sungwoo Lee, Seunghyeong Lee, Mihyang Park, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Diabetes & Metabolism Journal.2019; 43(6): 830. CrossRef - Recent advances in the pathogenesis of microvascular complications in diabetes
Sungmi Park, Hyeon-Ji Kang, Jae-Han Jeon, Min-Ji Kim, In-Kyu Lee
Archives of Pharmacal Research.2019; 42(3): 252. CrossRef - Diabetic nephropathy: An update on pathogenesis and drug development
Vikram Rao A/L B Vasanth Rao, Sean Hong Tan, Mayuren Candasamy, Subrat Kumar Bhattamisra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 754. CrossRef - Mechanisms and pathways of anti‐inflammatory activity of DPP‐4 inhibitors in cardiovascular and renal protection
Katarina Tomovic, Jelena Lazarevic, Gordana Kocic, Marina Deljanin‐Ilic, Marko Anderluh, Andrija Smelcerovic
Medicinal Research Reviews.2019; 39(1): 404. CrossRef - Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2019; 34(1): 80. CrossRef - The emerging role of novel antihyperglycemic agents in the treatment of heart failure and diabetes: A focus on cardiorenal outcomes
Kelly R. McHugh, Adam D. DeVore, Robert J. Mentz, Daniel Edmonston, Jennifer B. Green, Adrian F. Hernandez
Clinical Cardiology.2018; 41(9): 1259. CrossRef - Acute Kidney Injury and Progression of Diabetic Kidney Disease
Samuel Mon-Wei Yu, Joseph V. Bonventre
Advances in Chronic Kidney Disease.2018; 25(2): 166. CrossRef - Recombinant human GLP-1(rhGLP-1) alleviating renal tubulointestitial injury in diabetic STZ-induced rats
Weiqin Yin, Shiqing Xu, Zai Wang, Honglin Liu, Liang Peng, Qing Fang, Tingting Deng, Wenjian Zhang, Jinning Lou
Biochemical and Biophysical Research Communications.2018; 495(1): 793. CrossRef - Chronic inhalation of e-cigarette vapor containing nicotine disrupts airway barrier function and induces systemic inflammation and multiorgan fibrosis in mice
Laura E. Crotty Alexander, Christopher A. Drummond, Mark Hepokoski, Denzil Mathew, Alex Moshensky, Andrew Willeford, Soumita Das, Prabhleen Singh, Zach Yong, Jasmine H. Lee, Kevin Vega, Ashley Du, John Shin, Christian Javier, Jiang Tian, Joan Heller Brown
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2018; 314(6): R834. CrossRef - Renoprotective effect of fucoidan from Acaudina molpadioides in streptozotocin/high fat diet-induced type 2 diabetic mice
Shiwei Hu, Jinhui Wang, Jingfeng Wang, Shijie Li, Wei Jiang, Yu Liu
Journal of Functional Foods.2017; 31: 123. CrossRef - Dipeptidyl peptidase-4 inhibition and renoprotection
Yuta Takagaki, Daisuke Koya, Keizo Kanasaki
Current Opinion in Nephrology and Hypertension.2017; 26(1): 56. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Pharmacological Treatment in Diabetes Mellitus Type 1 – Insulin and What Else?
Ewa Otto-Buczkowska, Natalia Jainta
International Journal of Endocrinology and Metabolism.2017;[Epub] CrossRef - GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes
Marcel H. A. Muskiet, Lennart Tonneijck, Mark M. Smits, Michaël J.B. van Baar, Mark H. H. Kramer, Ewout J. Hoorn, Jaap A. Joles, Daniël H. van Raalte
Nature Reviews Nephrology.2017; 13(10): 605. CrossRef - Efficacy, safety and albuminuria‐reducing effect of gemigliptin in Korean type 2 diabetes patients with moderate to severe renal impairment: A 12‐week, double‐blind randomized study (the GUARD Study)
Sun A. Yoon, Byoung G. Han, Sung G. Kim, Sang Y. Han, Young I. Jo, Kyung H. Jeong, Kook H. Oh, Hyeong C. Park, Sun H. Park, Shin W. Kang, Ki R. Na, Sun W. Kang, Nam H. Kim, Young H. Jang, Seong H. Shin, Dae R. Cha
Diabetes, Obesity and Metabolism.2017; 19(4): 590. CrossRef - Sodium butyrate has context-dependent actions on dipeptidyl peptidase-4 and other metabolic parameters
Eun-Sol Lee, Dong-Sung Lee, Prakash Raj Pandeya, Youn-Chul Kim, Dae-Gil Kang, Ho-Sub Lee, Byung-Chul Oh, Dae Ho Lee
The Korean Journal of Physiology & Pharmacology.2017; 21(5): 519. CrossRef - Lobeglitazone, a Novel Peroxisome Proliferator-Activated Receptor γ Agonist, Attenuates Renal Fibrosis Caused by Unilateral Ureteral Obstruction in Mice
Kwi-Hyun Bae, Jung Beom Seo, Yun-A Jung, Hye-Young Seo, Sun Hee Kang, Hui-Jeon Jeon, Jae Man Lee, Sungwoo Lee, Jung-Guk Kim, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Endocrinology and Metabolism.2017; 32(1): 115. CrossRef - Gemigliptin: An Update of Its Clinical Use in the Management of Type 2 Diabetes Mellitus
Sung-Ho Kim, Jung-Hwa Yoo, Woo Je Lee, Cheol-Young Park
Diabetes & Metabolism Journal.2016; 40(5): 339. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef
- Diabetic fibrosis
- Letter: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (
Diabetes Metab J 2015;39:498-506) - Mi-Kyung Kim
- Diabetes Metab J. 2016;40(1):83-84. Published online February 19, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.1.83
- 2,669 View
- 25 Download
- Assessment of the Association between Mean Hemoglobin A1c Levels for 5 Years and Coronary Artery Disease by Coronary Angiography in Nondiabetic Patients
- Jae-Joon Kim, Ji-Hoon Kang, Ja-Jun Goo, Kyoung-Nyoun Kim, Ja-Young Lee, Mi-kyung Kim, Tae Ik Kim
- Diabetes Metab J. 2014;38(1):58-63. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.58
- 3,972 View
- 27 Download
- 4 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The effects of glucose on cardiovascular events or mortality in nondiabetic patients has been recently reported. However, since atherosclerosis can be formed over a long period of time, it is necessary to devote several years to unveil the relationship between the two factors. Here, we attempted to find out the relationship between the mean hemoglobin A1c (HbA1c) level and HbA1c variability for 5 years and coronary artery disease (CAD) by using coronary angiography (CAG) to assess nondiabetic patients.
Methods We reviewed patients who performed CAG who were followed up for at least 5 years after the initial diagnosis. The fasting blood test was performed annually for glucose and HbA1c level. CAD was defined as more than 50% of luminal narrowing. The severity of CAD was divided into two groups depending on whether no vessels were involved or one more vessel were involved (CAD(-) or CAD(+), respectively).
Results The patients in CAD(+) group had higher mean HbA1c level for 5 years than CAD(-) group (5.71±0.40 vs. 5.86±0.68;
P =0.04). Mean HbA1c was a significant predictor for CAD in multiple regression (odds ratio, 2.224;P =0.028). The percentage of patients with CAD was significantly higher in patients with >6.2% of mean HbA1c levels compared to patients with <6.2% of mean HbA1c levels (P <0.019).Conclusion When the mean HbA1c levels were above 6.2%, the risk of CAD was higher. Also this study shows that HbA1c level can be one of the predictors for CAD even if the patients do not have diabetes.
-
Citations
Citations to this article as recorded by- Impact of a comprehensive cardiac rehabilitation programme versus coronary revascularisation in patients with stable angina pectoris: study protocol for the PRO-FIT randomised controlled trial
Joyce M. Heutinck, Iris A. De Koning, Tom Vromen, Robert-Jan M. Van Geuns, Dick H.J. Thijssen, Hareld M.C. Kemps, Eddy M. Adang, Johanna M. Geleijnse, Pieter van Gorp, Arnoud W. J. van ‘t Hof, Veronica R. Janssen, Harald T. Jorstad, Roderik A. Kraaijenhag
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Evaluation of HbA1c as a prognostic biomarker of cardiovascular events and mortality in nondiabetic patients: Methodological considerations
Denis Monneret
Atherosclerosis.2015; 242(1): 19. CrossRef
- Impact of a comprehensive cardiac rehabilitation programme versus coronary revascularisation in patients with stable angina pectoris: study protocol for the PRO-FIT randomised controlled trial
- Relationship between Chemerin Levels and Cardiometabolic Parameters and Degree of Coronary Stenosis in Korean Patients with Coronary Artery Disease
- Yu-Jin Hah, Nam-Keong Kim, Mi-Kyung Kim, Hye-Soon Kim, Seung-Ho Hur, Hyuck-Jun Yoon, Yoon-Nyun Kim, Keun-Gyu Park
- Diabetes Metab J. 2011;35(3):248-254. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.248
- 24,770 View
- 30 Download
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Chemerin is a novel adipokine that is associated with inflammation and adipogenesis. However, it remains unclear whether chemerin is involved in patients with cardiovascular disease. We investigated whether the serum chemerin levels of Korean patients with coronary artery disease correlated with specific cardiometabolic parameters.
Methods In total, 131 patients, all of whom had coronary artery stenosis exceeding 50%, participated in this study. Their serum chemerin levels and cardiometabolic parameters were measured. The serum chemerin levels of two groups of patients were compared; those with one stenotic vessel (
n =68) and those with multiple stenotic vessels, including left main coronary artery disease (n =63).Results Serum chemerin levels correlated positively with the degree of coronary artery stenosis and fasting glucose, triglyceride, total cholesterol, low density lipoprotein cholesterol, and high sensitive C-reactive protein levels. The group with multiple stenotic vessels, including left main disease, had higher chemerin levels than the group with one stenotic vessel (
t =-2.129,P =0.035). Multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease (odds ratio, 1.018; confidence interval, 0.997 to 1.040;P =0.091).Conclusion Serum chemerin levels have a significant correlation with several cardiometabolic risk factors and the degree of coronary artery stenosis in Korean patients with coronary artery disease. However, multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease. Additional investigations are necessary to fully elucidate the role of chemerin in cardiovascular disease.
-
Citations
Citations to this article as recorded by- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia
Lunbo Tan, Zijun Ouyang, Zhilong Chen, Fen Sun, Haichun Guo, Feng Wang, Monique Mulder, Yuan Sun, Xifeng Lu, Jian V. Zhang, A. H. Jan Danser, Koen Verdonk, Xiujun Fan, Qing Yang
Lipids in Health and Disease.2023;[Epub] CrossRef - Chemerin Levels in Acute Coronary Syndrome: Systematic Review and Meta-Analysis
Abdulrahman Ismaiel, Mohammad Zeeshan Ashfaq, Daniel-Corneliu Leucuta, Mohamed Ismaiel, Dilara Ensar Ismaiel, Stefan-Lucian Popa, Dan L Dumitrascu
Laboratory Medicine.2022; 53(6): 552. CrossRef - Prognostic value of plasma adipokine chemerin in patients with coronary artery disease
Bo Wang, Wenxin Kou, Shuya Ji, Rongrong Shen, Hongwei Ji, Jianhui Zhuang, Yifan Zhao, Bo Li, Wenhui Peng, Xuejing Yu, Hailing Li, Yawei Xu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Role of Chemerin in Cardiovascular Diseases
Mirjana T. Macvanin, Manfredi Rizzo, Jelena Radovanovic, Alper Sonmez, Francesco Paneni, Esma R. Isenovic
Biomedicines.2022; 10(11): 2970. CrossRef - Chemerin in inflammatory diseases
Xin Su, Ye Cheng, Guoming Zhang, Bin Wang
Clinica Chimica Acta.2021; 517: 41. CrossRef - Chemerin activity in selected pathological states of human body – A systematic review
Magdalena Acewicz, Irena Kasacka
Advances in Medical Sciences.2021; 66(2): 270. CrossRef - Chemerin in atherosclerosis
Jia-Xiang Sun, Chi Zhang, Zhe-Bin Cheng, Mu-Yao Tang, Yi-Zhang Liu, Jie-Feng Jiang, Xuan Xiao, Liang Huang
Clinica Chimica Acta.2021; 520: 8. CrossRef - Serum Chemerin Concentration Is Associated with Proinflammatory Status in Chronic Coronary Syndrome
Anna Szpakowicz, Malgorzata Szpakowicz, Magda Lapinska, Marlena Paniczko, Slawomir Lawicki, Andrzej Raczkowski, Marcin Kondraciuk, Emilia Sawicka, Malgorzata Chlabicz, Marcin Kozuch, Maciej Poludniewski, Slawomir Dobrzycki, Irina Kowalska, Karol Kaminski
Biomolecules.2021; 11(8): 1149. CrossRef - Novo Efeito Cardioprotetor da L-Carnitina em Camundongos Obesos Diabéticos: Regulação da Expressão de Quemerina e CMKLRI no Coração e Tecidos Adiposos
Rezvan Amiri, Mohammad Reza Tabandeh, Seyed Ahmad Hosseini
Arquivos Brasileiros de Cardiologia.2021; 117(4): 715. CrossRef - The role of adipokines in the regulation of cardiovascular function
A. V. Karpushev, V. B. Mikhailova
"Arterial’naya Gipertenziya" ("Arterial Hypertension").2020; 25(5): 448. CrossRef - The associations among RARRES2 rs17173608 gene polymorphism, serum chemerin, and non-traditional lipid profile in patients with metabolic syndrome
Marwa A. Dahpy, Marwa K. Khairallah, Nashwa Mostafa A. Azoz, Ghada M. Ezzat
Egyptian Journal of Medical Human Genetics.2020;[Epub] CrossRef - Serum chemerin as a predictor of left ventricle hypertrophy in patients with coronary artery disease
NohaHasssanin Hanboly, Yasser Sharaf, Mervat Al-Anany, Essam Saeed
Nigerian Journal of Cardiology.2019; 16(1): 25. CrossRef - Association of Circulating Chemerin With Subclinical Parameters of Atherosclerosis
Stephanie Zylla, Marcus Dörr, Henry Völzke, Ulf Schminke, Stephan B. Felix, Matthias Nauck, Nele Friedrich
Arteriosclerosis, Thrombosis, and Vascular Biology.2018; 38(7): 1656. CrossRef - Six weeks of combined aerobic and resistance exercise using outdoor exercise machines improves fitness, insulin resistance, and chemerin in the Korean elderly: A pilot randomized controlled trial
Dong-Il Kim, Dong Hoon Lee, Sunghyun Hong, Sung-won Jo, Young-shin Won, Justin Y. Jeon
Archives of Gerontology and Geriatrics.2018; 75: 59. CrossRef - Relationship between serum chemerin levels and insulin resistance index and cardio–respiratory function in non–active obese and lean men
Mehdi Abbaszadegan, Farhad Kouhi achachluie
Advances in Obesity, Weight Management & Control.2018;[Epub] CrossRef - Serum levels of chemerin, apelin, vaspin, and omentin-1 in obese type 2 diabetic Egyptian patients with coronary artery stenosis
Tarek M.K. Motawi, Soliman G. Mahdy, Maha M. El-Sawalhi, Eman N. Ali, Rania Farag A. El-Telbany
Canadian Journal of Physiology and Pharmacology.2018; 96(1): 38. CrossRef - Plasma CXCL1 levels and TRAF3IP2 variants in patients with myocardial infarction
Safoora Pordel, Mahdi Sajedi Khanian, Mohammad Hossein Karimi, Hossein Nikoo, Mehrnoosh Doroudchi
Journal of Clinical Laboratory Analysis.2018;[Epub] CrossRef - Serum Chemerin Levels are Associated with Visceral Adiposity, Independent of Waist Circumference, in Newly Diagnosed Type 2 Diabetic Subjects
Dae Young Cheon, Jun Goo Kang, Seong Jin Lee, Sung Hee Ihm, Eun Jig Lee, Moon Gi Choi, Hyung Joon Yoo, Chul Sik Kim
Yonsei Medical Journal.2017; 58(2): 319. CrossRef - The comparison of chemerin, adiponectin and lipid profile indices in obese and non-obese adolescents
Zahra Maghsoudi, Roya Kelishadi, Mohammad Javad Hosseinzadeh-Attar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2016; 10(2): S43. CrossRef - Chemerin processing in the myocardium: A mechanism in search of a function
Michael V.G. Latronico, Gianluigi Condorelli
Journal of Molecular and Cellular Cardiology.2016; 100: 21. CrossRef - Chemerin as an independent predictor of cardiovascular event risk
Sinan İnci, Gökhan Aksan, Pınar Doğan
Therapeutic Advances in Endocrinology and Metabolism.2016; 7(2): 57. CrossRef - Chemerin level in pregnancies complicated by preeclampsia and its relation with disease severity and neonatal outcomes
Orkun Cetin, Zehra Kurdoglu, Mertihan Kurdoglu, H. Guler Sahin
Journal of Obstetrics and Gynaecology.2016; : 1. CrossRef - Chemerin in renal dysfunction and cardiovascular disease
Mario Bonomini, Assunta Pandolfi
Vascular Pharmacology.2016; 77: 28. CrossRef - High plasma chemerin is associated with renal dysfunction and predictive for cardiovascular events — Insights from phenotype and genotype characterization
Andreas Leiherer, Axel Muendlein, Elena Kinz, Alexander Vonbank, Philipp Rein, Peter Fraunberger, Cornelia Malin, Christoph H. Saely, Heinz Drexel
Vascular Pharmacology.2016; 77: 60. CrossRef - Chemerin plays a protective role by regulating human umbilical vein endothelial cell-induced nitric oxide signaling in preeclampsia
Liqiong Wang, Tianli Yang, Yiling Ding, Yan Zhong, Ling Yu, Mei Peng
Endocrine.2015; 48(1): 299. CrossRef - Evaluation of the salivary levels of visfatin, chemerin, and progranulin in periodontal inflammation
Erkan Özcan, N. Işıl Saygun, Muhittin A. Serdar, Nezahat Kurt
Clinical Oral Investigations.2015; 19(4): 921. CrossRef - Elevated serum chemerin in Chinese women with hyperandrogenic PCOS
LiQiong Wang, Yan Zhong, YiLing Ding, XiaoBo Shi, Jian Huang, FuFan Zhu
Gynecological Endocrinology.2014; 30(10): 746. CrossRef - Chemerin reduces vascular nitric oxide/cGMP signalling in rat aorta: a link to vascular dysfunction in obesity?
Karla Bianca Neves, Núbia S. Lobato, Rhéure Alves Moreira Lopes, Fernando P. Filgueira, Camila Ziliotto Zanotto, Ana Maria Oliveira, Rita C. Tostes
Clinical Science.2014; 127(2): 111. CrossRef - Chemerin levels as predictor of acute coronary events: A case–control study nested within the veterans affairs normative aging study
Konstantinos N. Aronis, Ayse Sahin-Efe, John P. Chamberland, Avron Spiro, Pantel Vokonas, Christos S. Mantzoros
Metabolism.2014; 63(6): 760. CrossRef - The predictive value of the first-trimester maternal serum chemerin level for pre-eclampsia
Qiu-Lian Xu, Min Zhu, Yan Jin, Nan Wang, Hai-Xia Xu, Li-Mei Quan, Shan-Shan Wang, Shan-Shan Li
Peptides.2014; 62: 150. CrossRef - Evaluation of Circulating Adipokines and Abdominal Obesity as Predictors of Significant Myocardial Ischemia Using Gated Single-Photon Emission Computed Tomography
Chi-Sheng Hung, Yen-Wen Wu, Jei-Yie Huang, Pei-Ying Hsu, Ming-Fong Chen, Xin-Liang Ma
PLoS ONE.2014; 9(5): e97710. CrossRef - Towards an integrative approach to understanding the role of chemerin in human health and disease
J. L. Rourke, H. J. Dranse, C. J. Sinal
Obesity Reviews.2013; 14(3): 245. CrossRef - The association between chemerin and homeostasis assessment of insulin resistance at baseline and after weight reduction via lifestyle modifications in young obese adults
Mi Kyung Lee, Sang Hui Chu, Duk Chul Lee, Ki Yong An, Ji-Hye Park, Dong Il Kim, Jiyoung Kim, Sunghyun Hong, Jee Aee Im, Ji Won Lee, Justin Y. Jeon
Clinica Chimica Acta.2013; 421: 109. CrossRef - Elevated Chemerin Levels in Pakistani Men: An Interrelation with Metabolic Syndrome Phenotypes
Syeda Sadia Fatima, Kiymet Bozaoglu, Rehana Rehman, Faiza Alam, Abdul Shakoor Memon, Pascale Chavatte-Palmer
PLoS ONE.2013; 8(2): e57113. CrossRef - Chemerin: a potential endocrine link between obesity and type 2 diabetes
Alexandra A. Roman, Sebastian D. Parlee, Christopher J. Sinal
Endocrine.2012; 42(2): 243. CrossRef - Elastase and Tryptase Govern TNFα-Mediated Production of Active Chemerin by Adipocytes
Sebastian D. Parlee, Jenna O. McNeil, Shanmugam Muruganandan, Christopher J. Sinal, Kerry B. Goralski, Charaf Benarafa
PLoS ONE.2012; 7(12): e51072. CrossRef - Potential association between coronary artery disease and the inflammatory biomarker YKL-40 in asymptomatic patients with type 2 diabetes mellitus
Hyun Min Kim, Byung-Wan Lee, Young-Mi Song, Won Jin Kim, Hyuk-Jae Chang, Dong-Hoon Choi, Hee Tae Yu, EunSeok Kang, Bong Soo Cha, Hyun Chul Lee
Cardiovascular Diabetology.2012;[Epub] CrossRef - The association of serum chemerin level with risk of coronary artery disease in Chinese adults
Qun Yan, Yifei Zhang, Jie Hong, Weiqiong Gu, Meng Dai, Juan Shi, Ying Zhai, Weiqing Wang, Xiaoying Li, Guang Ning
Endocrine.2012; 41(2): 281. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef - Chemerin: A Novel Link between Inflammation and Atherosclerosis?
Eun-Jung Rhee
Diabetes & Metabolism Journal.2011; 35(3): 216. CrossRef
- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia

 KDA
KDA
 First
First Prev
Prev





